PETALING JAYA: While awareness of cervical cancer in Malaysia is generally high among women, participation in screening and preventive programmes remains low.
Recent findings by the Women, Family and Community Development Ministry show that it is the third most common form of cancer for women, compared with a 2020 World Health Organisation (WHO) survey that put it at fourth place.
Despite the high incidence, there are many women who have never gone for a pap smear, a procedure to detect cervical cancer.
Consultant obstetrician and gynaecologist Dr John Teo attributed the low figure to embarrassment with such an intimate procedure as well as the fear of bad news.
“Some are also afraid that it could be painful while others have the attitude that cancer ‘only affects others’.”
He said such barriers can be overcome with the use of modern methods such as the human papillomavirus (HPV) self-screening procedure.
“A national screening programme with a call and recall system, coupled with sustained efforts by stakeholders to dispel the myths and misconceptions about pap smears or HPV, can help to increase cervical screening.”
Teo added that there are also other concerns, such as unmarried women who seek contraception being open to stigmatisation and discrimination.
“To address this, healthcare professionals can be put through ‘sensitisation’ training so they learn to not only empathise with the patient but not judge them either. This should be part and parcel of the training in primary healthcare.”
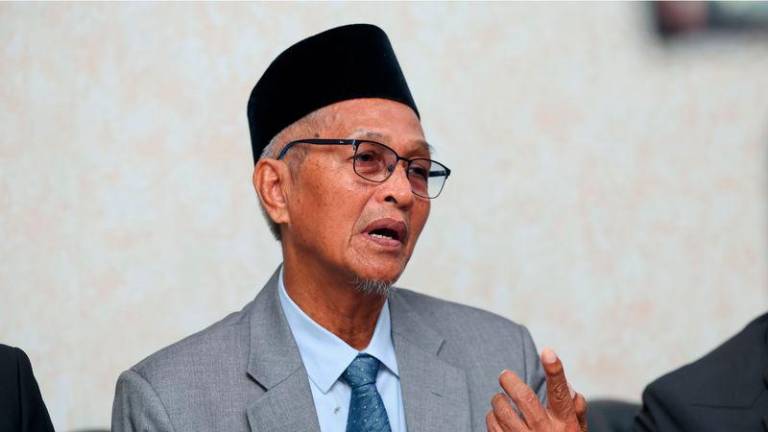
Obstetrics and gynaecology specialist Dr Badrul Zaman Abdullah, who is also a member of the Malaysian Gynaecologic Cancer Society, said women should get to know the criteria that qualify them for a free pap smear at a public healthcare facility.
“Today, women aged 30 to 65 who are sexually active are eligible for a pap smear at a public healthcare facility or family planning clinic,” he told theSun.
Initially, it was done at two-year intervals and if the results do not show any signs of cancer, it can be extended to three years between procedures.
Badrul Zaman said women aged 30 to 65 who have had sexual intercourse but have not had a pap smear for three years and never had a HPV would also be eligible for a HPV self-test.
He said a woman is entitled to a free pap smear or HPV if she meets all the given criteria, whether or not she is married.
“Generally, being unmarried is not a prerequisite exclusion criteria if other risk factors are detected. A trained doctor would usually assess all of a patient’s risk factors and background medical profile,” he said.
“Medical advice is likely evidence-based and women should be empowered to make informed decisions in regard to their sexual health and well being.”
Badrul Zaman added that women should not rely solely on a pap smear.
“Efforts to overcome and eliminate cervical cancer comes in the form of HPV vaccination, HPV testing (self-sampling or by a healthcare provider) as well as treatment of cervical disease,” he said.
This triple intervention outlined by WHO is part of a global effort for the elimination of cervical cancer, with a threshold target of less than four cases per 100,000 women.
Badrul Zaman said HPV self-testing seems to be the key to removing obstacles to cervical cancer screening.
“The lifetime risk of Malaysian women to have cervical cancer is one in 144. The incidence increases after 35 years of age and peaks between 54 to 65 years of age. Some 59% of these cancer patients are presently at stage one and two, despite the screening modalities available.”