THE most common food allergy among infants is cow’s milk protein allergy (CMPA). This occurs when an infant consumes or comes into contact with cow’s milk and its products. The child’s immune system reacts abnormally to the protein in cow’s milk and attempts to neutralise the protein by releasing various chemicals causing the symptoms of CMPA.
It is estimated to affect between 5-8% of infants worldwide. CMPA typically begins in the first few months of life, although they may not immediately develop symptoms upon the first few consumption of milk. Generally, the majority of children outgrow CMPA where 50% outgrow it by age 1-2 years, 80% by 4 years, and 90% by 6 years of age. However certain groups of children especially those with other allergic conditions including asthma, rhinitis, or eczema, are at higher risk of persistent CMPA symptoms.
The allergic reactions can be classified into rapid onset which occurs within an hour of ingestion, or delayed onset which takes hours to days to develop the symptoms. The symptoms may affect various body systems including the gastrointestinal, skin, and respiratory systems. Some of the typical symptoms are skin hives, swelling of the face and throat, coughing or shortness of breath, wheezing, and diarrhoea. On rare occasions, anaphylaxis may occur, which is a medical emergency requiring immediate treatment.
CMPA is sometimes confused with lactose intolerance. However, lactose intolerance does not involve the immune system and generally present with bloating or diarrhoea after consuming milk or lactose-containing foods. Lactose intolerance occurs when the digestive system is not able to fully digest lactose. It is important to differentiate the two as the treatment are different.
Diagnosis is primarily based on the history of the symptoms and there are no specific tests. The gold standard for diagnosis is the oral food challenge, whereby if the symptoms improve following the elimination of cow’s milk in the diet, the diagnosis is better supported. Sometimes certain allergic tests including a skin prick test and blood test to measure specific IgE antibodies may be helpful.
If you suspect your child may have CMPA, it is best to consult your doctor to confirm the diagnosis rather than to immediately attempt to eliminate or substitute cow’s milk in your child’s diet.
Once confirmed, the key principle in the treatment of CMPA is the elimination of cow’s milk from the infant’s diet. Infants who can be fully breastfed and children above the age of 2 years who no longer need to depend on formula milk may not need any substitute formula milk.
Avoiding cow’s milk is not limited to the infant only consuming milk. Exposure to cow’s milk can also occur from inhaling or by touch and can also lead to developing symptoms.
In searching for substitute formulas, several options are available. It is important to note that goat’s milk-based formula is not recommended as a substitute due to the high chances of cross-reactivity where the infant may also have a reaction to the milk. Goat’s milk is also high in sodium and low in folic acid thus increasing the risk of nutritional imbalances in the infant.

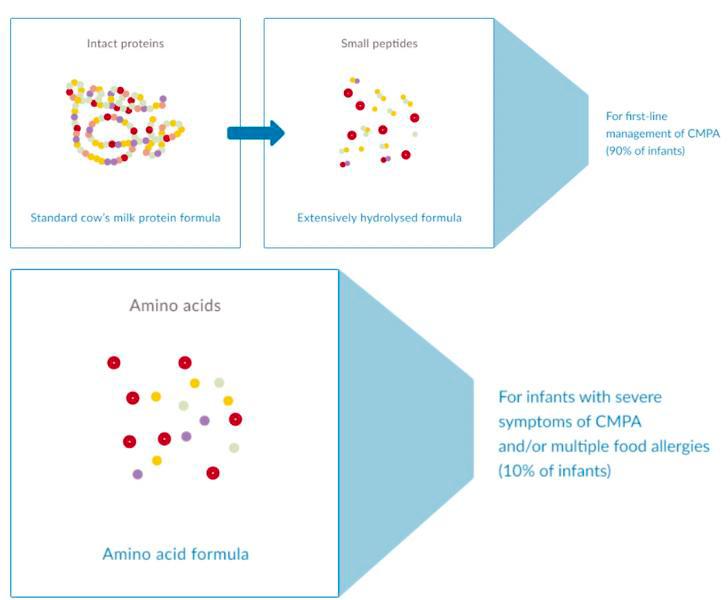
Whenever possible, it is best to continue fully breastfeeding and stop giving formula milk to the infant. If this is not possible, the preferred option is to use extensively hydrolysed formula (EHF). In EHF, the cow’s milk protein is broken down into smaller peptides making them less allergenic as compared to whole cow’s milk protein. In severe cases, the use of amino acid formula (AAF) is recommended where the protein chain is further broken down into simple amino acids.
The disadvantage of using EHF and AAF are that they have a less palatable taste as compared to normal infant formula. They are also more expensive and may not be as easily available.
EHF and AAF are not to be confused with another available type of formula named partially hydrolysed formula (PHF) which has a slightly shorter protein chain. PHF may still cause CMPA reactions and is not recommended in the treatment of CMPA.
For infants above 6 months old, sometimes soy-based formula may be given instead. However there have been some reports of cross-reactivity to soy-based formula, and soy formula is not recommended for use with preterm babies and cannot be given to babies who have conditions such as galactosaemia.
An interesting point of study is the use of hydrolysed formula in preventing the occurrence of allergies in the child. So far, there is still yet to be concrete and consistent evidence to support the use of hydrolysed formula in preventing allergies.
There are however some studies that suggest that the risk of developing eczema may be lower in the group consuming the hydrolysed formula. As a whole, using hydrolysed formula milk in preventing allergies cannot be confidently advised.
Dr Yeap is a paediatrician attached to KPJ Sentosa KL. Through his articles, he aims to help increase public awareness of the common issues associated with children’s health.










